Krishna Pundi, MD
Mintu Turakhia, MD MS
Michael Wurm, Head of Product
Executive Summary
Remote patient monitoring (RPM) has grown rapidly in U.S. health care practices and health care systems. In 2019, the Centers for Medicare & Medicaid Services implemented monthly reimbursement for medical device supply and training, data transmission, and clinical evaluation of RPM. Although the COVID-19 pandemic was a strong force behind the rapid adoption and implementation of RPM, a large body of evidence demonstrates its ability to expand access to care and improve health outcomes while reducing costs.
Since its RPM product launch in June 2019, 100Plus RPM has serviced over 30,000 patients in 426 health care practices. In this white paper, we examine the trends of 100Plus RPM patients in three key metrics: weight, blood glucose, and blood pressure. In addition, we review the results of health care provider surveys on the impact of 100Plus RPM on patient care and discuss the potential effects on health outcomes and costs.
Mean Improvement in Clinical Parameters Over Patients’ First 180 days

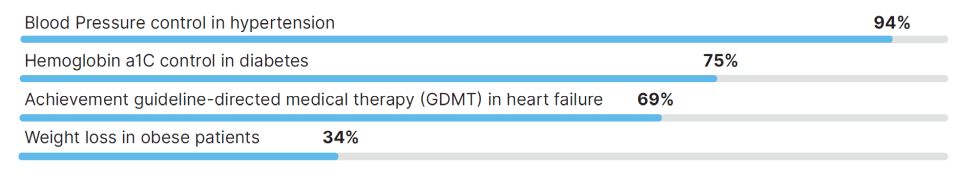
Percentage of providers who assert 100Plus has improved or greatly improved…
Introduction
Remote patient monitoring (RPM) comprises a broad set of strategies that acquire physiologic and disease-related data from a user’s home and deliver them to health care providers. Between 2003 and 2013, early RPM technologies demonstrated the ability to reduce hospitalizations and morbidity.¹ In 2018, the University of Pittsburgh Medical Center equipped their patients with digital tablets and RPM devices to reduce hospital readmission risk by 76%; patient satisfaction exceeded 90% in RPM patients. Recognizing the potential benefits of RPM, the Centers for Medicare & Medicaid Services introduced five separate CPT codes for the use and monitoring of RPM since 2018, providing health care providers the financial support to integrate RPM into their practices.
With the rising need for consumer-friendly remote monitoring, 100Plus RPM was introduced in 2019 with an explicit goal of reducing patient, clinician, and health care system barriers to RPM use. 100Plus developed an RPM system that:
- Requires minimal time from clinicians to enroll, educate, provision, and train patients.
- Gives patients a zero-setup experience where devices work out of the box without any pairing or connectivity setup, and app-less support and engagement via text message, which has 92% reach among seniors and 98% open rate.
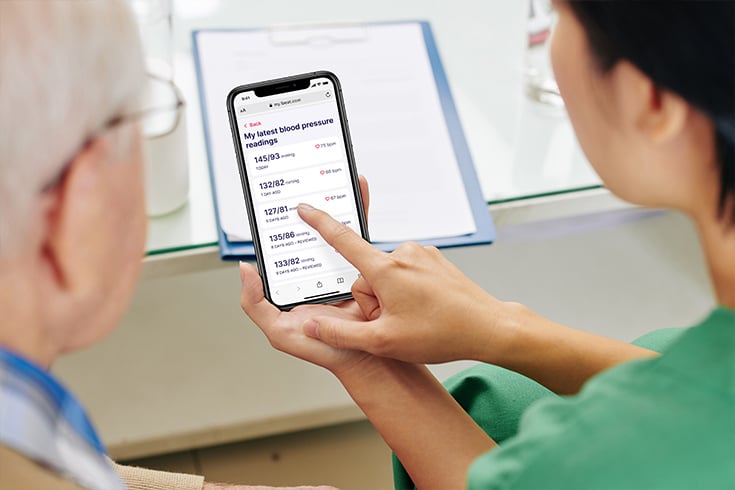
- Offers an easy to use patient portal that enables patients to view their readings history, and provides confirmation that a clinician has received their data, and is monitoring their progress.
- Gives clinicians simple patient dashboards, and accurate, streamlined reimbursement.
- Provides full-service patient data monitoring and billing support.
How Does Remote Patient Monitoring Work With 100Plus?
- Eligibility Verification: Confirm RPM-eligible patients.
- Enrollment and Onboarding: Reduce the burden on your clinicians and staff.
- Adherence and Population Health Management: Accelerated by Esper, your AI-based virtual health assistant.
- Billing and Reimbursement: Track and submit time spent to know when Medicare requirements are met and you are reimbursemed each month.
- Ongoing Patient Data Monitoring: Prioritize patient care and minimize workload.
For patients, 100Plus RPM devices are shipped fully configured and ready to use when they are delivered directly to a patient’s home. Esper, an AI-enabled virtual medical assistant who engages with patients via SMS then prompts the patient to unbox their devices, watch a quick onboarding video, and take their first reading. When patients text Esper questions, she responds in the moment with salient videos and escalation options as necessary.
Once patients take their reading, the device sends the data encrypted over cellular connection to their clinician’s EHR for ease of review, intervention, and billing. Esper texts positive reinforcement to patients upon streaks of daily readings. When patients fall out of adherence, Esper encourages them to take a reading via her accrued sense of personal connection and accountability with the patient. Esper also meets patients where they are in their complex lives, pausing reminders and following up once they are available to take a reading.
Quality Improvement Analysis
As adoption of 100Plus RPM has continued to expand, we performed an internal quality analysis to (1) determine the impact of the 100Plus RPM system on key health metrics and (2) evaluate health care provider perspectives on how it has affected care delivery.
Methodology
We performed retrospective quality improvement and quality assurance analysis of 100Plus RPM patients. We used an aggregated, de-identified dataset for internal quality review of all 100Plus RPM patients starting from our launch date June 1, 2019 until October 21, 2022.
We also performed a clinician and practice survey to understand the impact of 100Plus RPM on individual practices. Health care providers at participating practices were sent a 15-question survey electronically. Responding practices were not provided any monetary compensation for their responses.
In the patient quality analysis, there were 426 practices across 43 states using 100Plus RPM, accounting for 31,102 patients. Among these patients, 59.5% were women, the median age was 73±12 years among female patients, and 73±12 years among male patients. Data regarding patients’ weights, blood pressures, and blood glucose control were directly transmitted.
We focused on three key metrics: (1) blood pressure control, (2) blood glucose control in diabetic patients, and (3) weight loss in patients who weighed > 220 lbs and > 286 lbs. For statistical comparisons of repeated measures, we used t-tests to compare baseline values (day 0) to evaluate change in parameters at 90 days and 180 days. P values of < 0.05 were considered statistically significant.
Blood Pressure Control – From Hypertension to Heart Failure
Based on current population prevalence estimates, nearly 1 in 2 Americans have or will be diagnosed with hypertension in their lifetime.² Large clinical trials have also established a near-linear association between higher blood pressures and cardiovascular disease risk. While effective medications exist to treat hypertension, health care providers are often dependent on home blood pressure monitoring (HBPM) to account for factors such as dietary changes, varying medication effects and evaluate for masked or white coat hypertension.²⁄³
The American Heart Association (AHA) recognizes that RPM can serve as a vital conduit for improving hypertension control and reducing the economic burden that stems from the costly hospitalizations and events related to hypertension. A study published by the AHA found that for individuals with uncontrolled hypertension, remote monitoring may cut heart attack and stroke rates by 50%, compared to usual care and self-monitoring alone.⁴
 Hypertension Management with 100Plus
Hypertension Management with 100Plus
In total, there were 18,000 individuals using 100Plus RPM for the management of hypertension. The 8,428 hypertensive patients with an initial RPM systolic blood pressure reading of >140 mmHg saw their mean systolic blood pressure drop by 16.0 mmHg from 157.2 to 141.2 mmHg over 180 days; those patients’ diastolic blood pressure dropped 8.9 mmHg from 86.8 to 77.9 mmHg (p < 0.0001). Across all 18,000 patients using 100Plus RPM for HBPM, the mean systolic blood pressure decreased by 3.5 mmHg from 139.5±21 mmHg to 136±20 mmHg over 180 days (p < 0.0001). Patients’ diastolic BP dropped proportionately, with the same sample size and statistical significance. By comparison, in a review of randomized controlled trials of RPM devices, HBPM resulted in a mean 1 mmHg reduction of systolic blood pressures in the intervention arms across five studies.⁵ However, we did not have a control arm of RPM non-patients and this was a quality improvement analysis, not a clinical study.
It is estimated that annual medical costs for hypertensive individuals are $1,920-$2,500 higher than non-hypertensive individuals, much of which could be reduced with more consistent hypertension management.⁶⁄⁷ HBPM as part of an integrated treatment strategy for hypertension provides a reduction in cardiovascular events while simultaneously creating cost-savings.⁸⁄⁹ By providing easy access HBPM and integrating seamlessly with health care provider workflow, 100Plus RPM can be a key component of the treatment strategy.
When surveyed, 94% of health care providers reported that 100Plus RPM improved or greatly improved blood pressure control. Additionally, 69% reported an improved ability to achieve guideline-directed medical therapy for heart failure.
For individuals with heart failure, initiation of guideline-directed medical therapy with appropriate increases in medication dosages leads to a reduction in heart failure hospitalization and death.¹⁰ However, in real-world populations, many patients are either not started on these medications or left on low doses, limiting overall treatment benefit.¹¹ A recent systematic review demonstrated that an individual with heart failure’s annual medical costs were approximately $24,383, primarily driven by heart failure hospitalizations.¹² Individuals with heart failure hospitalizations are also at high risk of readmission to the hospital within 30 days, with an added estimated cost of $15,732 – $25,879 per person.¹³ If health care providers are able to leverage 100Plus RPM to achieve guideline-directed medical therapy for heart failure and proactively make medication changes in the ambulatory setting, there is potential to avoid costly and morbid hospitalizations for heart failure.
Weight Management Is Challenging – But Rewarding
Obesity is a well-established risk factor for multiple medical conditions, including hypertension, hyperlipidemia, type 2 diabetes, cardiovascular disease, and fatty liver disease. In 2018, the CDC estimated that 42% of the US adult population was obese. Overall, obesity is estimated to add $3,559 in annual medical costs per person compared to those not obese.¹⁴ Weight loss has been a major focus of public and private health initiatives, and American and European professional society guidelines recommend weight monitoring as a critical component of behavioral and lifestyle changes for weight management.¹⁵⁄¹⁶
 High-risk 100Plus Users Demonstrated Weight Loss
High-risk 100Plus Users Demonstrated Weight Loss
1,767 patients had initial weight > 220lbs. 180 days after they started using 100Plus RPM, mean weight decreased by 7.3 lbs, from 257±34 lbs to 250±38 lbs (p < 0.0001). Weight loss was more pronounced for the 259 patients who had an initial weight > 286 lbs. 180 days after they started using 100Plus RPM, mean weight decreased by 12.1 lbs from 319±30 lbs to 307±41 lbs (p < 0.0001). In a subsequent survey, 34% of health care providers asserted that using 100Plus RPM improved or greatly improved weight loss for their patients with obesity.
Weight loss is inherently challenging for various physiologic, socioeconomic, and psychological reasons, yet even moderate changes in weight can have dramatic health and economic impacts. In a 50- year-old individual, just a shift from the “obese” to “overweight” category can reduce lifetime health care costs by approximately $20,000.¹⁷
While the observed weight loss in these individuals is not compared to a control group of non-users, the RPM platform plausibly creates an environment to facilitate weight loss. In 2016, a randomized controlled trial of the smartphone application Noom demonstrated that weight loss effects were more pronounced in individuals who monitored their weight frequently.¹⁸ In the Fogg Behavioral Model, motivation and ability synergize with an effective trigger to elicit behavioral change. For patients of 100Plus RPM, the act of daily weight measurement and interaction with Esper creates an environment of motivation and accountability. This combines with provider-based education on diet and activity changes to empower patients to make durable lifestyle changes and lose weight.
Diabetes Control – New Solutions for an Old Problem
Diabetes is a highly prevalent and growing problem for Americans – per the 2020 CDC National Diabetes Statistics Report, 34 million Americans are estimated to have diabetes, with an additional 88 million adults having pre-diabetes. Additionally, the direct and indirect effects of diabetes lead to a higher risk of vision problems, kidney failure, heart disease, stroke, and death. As of 2017, the American Diabetes Association estimated that $1 in every $7 spent on health care is in treating diabetes and its complications; overall, individuals with diabetes incur medical expenses 2.3 times higher than those who do not.¹⁹
The treatment of patients with diabetes primarily focuses on the management of blood glucose levels and long-term weight loss.²⁰ Self-monitoring of blood glucose has been an integral part of multifactorial approaches to diabetes control for its ability to guide nutrition and physical activity, prevent hypoglycemia, and help medication management.²¹ More frequent self monitoring has also been associated with lower Hemoglobin A1C levels, a marker of diabetic control.²²
 Glycemic Control in 100Plus Users With diabetes
Glycemic Control in 100Plus Users With diabetes
Overall, there were 4,989 patients of 100Plus RPM who had a history of diabetes and were using 100Plus RPM for glucose management. Over their first 180 days on the platform, patients mean random glucose decreased by 9.3 mg/dL from 153±70 mg/dL to 144±62 mg/dL (p < 0.0001). While glucometers do not measure hemoglobin A1C, which is considered the gold standard of measurement for long-term diabetic glucose control, 75% of surveyed providers asserted that 100Plus RPM improved or greatly improved hemoglobin A1C control for their patients with diabetes.
While self-monitoring of blood glucose is not new to diabetes, uptake of new technologies can often be hampered by psychosocial and socioeconomic barriers.²³ For older adults or individuals with neurologic or visual complications of diabetes, multi-step device setup or ability to navigate Smartphone applications may be challenging. Nadia Hamad, LVN of Greenville Health care Associates, describes the benefits of the 100Plus Glucometer:
“The bulk of our patient population is the elderly. I appreciate the 100Plus Glucometer because of its ease of use, particularly the color screen, font size, automatic transmission and patient directives. Our patients can easily adapt the device for everyday use, allowing increased compliance resulting in more robust data points for diabetic management. The fact that the glucometer is covered as an RPM service also allows for the prompt delivery of the device along with its supplies, decreasing the hassle of formulary coverage issues.”
— Nadia Hamad, LVN, Greenville Health Care Associates
By removing these additional barriers to care, 100Plus RPM patients may be empowered to self-monitor their glucose levels and interface with their health care providers, which could in turn improve long-term health outcomes.
Conclusion
RPM is growing rapidly and can synergize with telemedicine and face-to-face care as a means of improving and extending patient health care. While CMS has provided financial incentives incorporating RPM, it holds potential for overall improvement of health outcomes and cost reduction at a health care system level. In this non-randomized, intervention-only, quality improvement analysis, we noted statistically significant and clinically meaningful reductions in weight, blood pressure, and blood glucose in 100Plus RPM patients. We additionally note that most health care providers reported 100Plus RPM improved or greatly improved their ability to manage these metrics. These findings could have major health and cost implications for health care systems and further underline the growing role of RPM.
The Effect of 100Plus on These Metrics Is Likely Multifactorial
On the patient side:
- The perception of being observed, combined with reminders and feedback from Esper, can create a sense of accountability.
- By regularly measuring, patients’ motivation to make healthier decisions in improving these biometrics may also increase.
For health care providers:
The availability of biometric data enables more clinically informed decision-making and care so that patients do not have to wait for follow-up visits or catastrophic events for initiation, escalation, or discontinuation of medical therapies. The data provides a means of earlier intervention, either remotely or as a return visit, to get ahead of common clinical problems such as the need for therapy escalation, change in therapy, or addressing of barriers to improve medication adherence and refill compliance.
- The RPM platform may reduce therapeutic inertia, allowing for more rapid titration of therapies, such as for hypertension and diabetes, over a shorter course of time than over months or longer if indexed to routine, rather
than data-driven, follow-up visits. - The 100Plus RPM Provider Portal provides summaries of individual and system-wide performance on health metrics, which empowers quality improvement initiatives.
- The 100Plus full-service clinical monitoring team and billing support reduces administrative burden and workload.
The culmination of these effects could underlie the observed reductions in weight, blood pressure, and blood glucose. Across large health care systems, we see the potential for improvements in health care outcomes and system-wide cost savings.
Download the Complete White Paper
Limitations
Our data have limitations due to their observational nature. These data are retrospective and part of a quality improvement analysis. These data are not from a clinical study. There is no control arm since all of the patients are enrolled in RPM. They are not compared to a nonintervention arm since we don’t have the ethical capacity to create one as a technology services provider. Also, participating patients and health care providers may be more engaged in health care than those who did not.
References
- Kitsiou S, Paré G, Jaana M. Effects of Home Telemonitoring Interventions on Patients With Chronic Heart Failure: An Overview of Systematic Reviews. J Med Internet Res. 2015;17:e63.
- Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA, Williamson JD, Wright JT. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:1269–1324.
- Franklin SS, Thijs L, Hansen TW, O’Brien E, Staessen JA. White-Coat Hypertension: New Insights From Recent Studies. Hypertension. 2013;62:982–987.
- https://www.ahajournals.org/doi/full/10.1161/HYPERTENSIONAHA.120.15492
- Noah B, Keller MS, Mosadeghi S, Stein L, Johl S, Delshad S, Tashjian VC, Lew D, Kwan JT, Jusufagic A, Spiegel BMR. Impact of remote patient monitoring on clinical outcomes: an updated meta-analysis of randomized controlled trials. npj Digital Med. 2018;1:20172.
- Centers for Disease Control and Prevention. Cost-Effectiveness of High Blood Pressure Interventions [Internet]. US Department of Health and Human Services; [cited 2021 Oct 16]. Available from: https://www.cdc.gov/chronicdisease/programs-impact/pop/high-blood-pressure.htm
- Kirkland EB, Heincelman M, Bishu KG, Schumann SO, Schreiner A, Axon RN, Mauldin PD, Moran WP. Trends in health care Expenditures Among US Adults With Hypertension: National Estimates, 2003–2014. JAHA [Internet]. 2018 [cited 2021 Oct 16];7. Available from: https://www.ahajournals.org/doi/10.1161/JAHA.118.008731
- Moran AE, Odden MC, Thanataveerat A, Tzong KY, Rasmussen PW, Guzman D, Williams L, Bibbins-Domingo K, Coxson PG, Goldman L. Cost-Effectiveness of Hypertension Therapy According to 2014 Guidelines. N Engl J Med. 2015;372:447–455.
- Arrieta A, Woods JR, Qiao N, Jay SJ. Cost–Benefit Analysis of Home Blood Pressure Monitoring in Hypertension Diagnosis and Treatment: An Insurer Perspective. Hypertension. 2014;64:891–896.
- Murphy SP, Ibrahim NE, Januzzi JL. Heart Failure With Reduced Ejection Fraction: A Review. JAMA. 2020;324:488.
- Greene SJ, Fonarow GC, DeVore AD, Sharma PP, Vaduganathan M, Albert NM, Duffy CI, Hill CL, McCague K, Patterson JH, Spertus JA, Thomas L, Williams FB, Hernandez AF, Butler J. Titration of Medical Therapy for Heart Failure With Reduced Ejection Fraction. Journal of the American College of Cardiology. 2019;73:2365–2383.
- Urbich M, Globe G, Pantiri K, Heisen M, Bennison C, Wirtz HS, Di Tanna GL. A Systematic Review of Medical Costs Associated with Heart Failure in the USA (2014–2020). PharmacoEconomics. 2020;38:1219–1236.
- Lahewala S, Arora S, Tripathi B, Panaich S, Kumar V, Patel N, Savani S, Dave M, Varma Y, Badheka A, Deshmukh A, Gidwani U, Gopalan R, Briasoulis A. Heart failure: Same-hospital vs. different-hospital readmission outcomes. International Journal of Cardiology. 2019;278:186–191.
- Cawley J, Meyerhoefer C. The medical care costs of obesity: An instrumental variables approach. Journal of Health Economics. 2012;31:219–230.
- Garvey WT, Mechanick JI, Brett EM, Garber AJ, Hurley DL, Jastreboff AM, Nadolsky K, Pessah-Pollack R, Plodkowski R. American Association of Clinical Endocrinologists and American College of Endocrinology Comprehensive Clinical Practice Guidelines For Medical Care of Patients with Obesity. Endocrine Practice. 2016;22:1–203.
- Yumuk V, Tsigos C, Fried M, Schindler K, Busetto L, Micic D, Toplak H. European Guidelines for Obesity Management in Adults. Obes Facts. 2015;8:402–424.
- Fallah-Fini S, Adam A, Cheskin LJ, Bartsch SM, Lee BY. The Additional Costs and Health Effects of a Patient Having Overweight or Obesity: A Computational Model: Costs/Health Effects of a Patient with Obesity. Obesity. 2017;25:1809–1815.
- Chin SO, Keum C, Woo J, Park J, Choi HJ, Woo J, Rhee SY. Successful weight reduction and maintenance by using a smartphone application in those with overweight and obesity. Sci Rep. 2016;6:34563.
- American Diabetes Association. Economic Costs of Diabetes in the U.S. in 2017. Dia Care. 2018;41:917–928.
- American Diabetes Association. 6. Glycemic Targets: Standards of Medical Care in Diabetes—2021. Dia Care. 2021;44:S73–S84.
- The Effect of Intensive Treatment of Diabetes on the Development and Progression of Long-Term Complications in Insulin-Dependent Diabetes Mellitus. N Engl J Med. 1993;329:977–986.
- Miller KM, Beck RW, Bergenstal RM, Goland RS, Haller MJ, McGill JB, Rodriguez H, Simmons JH, Hirsch IB, for the T1D Exchange Clinic Network. Evidence of a Strong Association Between Frequency of Self-Monitoring of Blood Glucose and Hemoglobin A1c Levels in T1D Exchange Clinic Registry Participants. Diabetes Care. 2013;36:2009–2014.
- Liberman A, Barnard K. Diabetes Technology and the Human Factor. Diabetes Technology & Therapeutics. 2019;21:S-138-S-147.
Access the Latest RPM News
Stay up to date with the latest news, articles and webinars about remote patient monitoring and telehealth.
"*" indicates required fields